Dental Implants: A Permanent Solution for Missing Teeth 🦷
When it comes to replacing missing teeth, dental implants are considered the gold standard. They are small, screw-shaped posts, typically made of titanium, that are surgically placed into the jawbone to serve as a secure root for a replacement tooth. This technology provides a permanent and stable foundation that feels and functions just like your natural teeth.
However, not all dental implants are created equal. The most suitable type of implant for a patient depends on a variety of factors, including the number of teeth to be replaced, their location, and the patient’s jawbone density. Understanding these different types of dental implants is crucial for making an informed decision about your oral health.
Types of Dental Implants: A Complete Guide
When it comes to replacing missing teeth, dental implants are considered the gold standard for their durability, stability, and natural appearance. They are a permanent and highly effective solution that restores the function and beauty of your smile. While all implants are designed to serve as a secure root for a replacement tooth, it is crucial to understand that not all implants are created equal. The most suitable type of implant for a patient depends on a variety of factors, including the number of teeth to be replaced, their location, and the patient’s jawbone density. Understanding these different types of dental implants is the first step in making an informed decision about your oral health.
1. Endosteal Implants
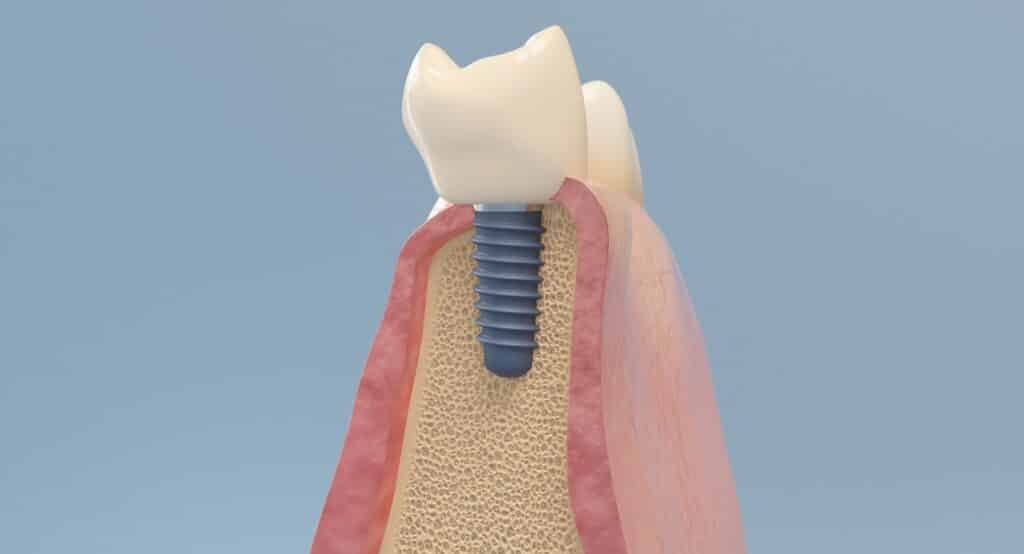
Endosteal implants are the most common type of dental implants used today. They are typically made of biocompatible materials like titanium and are shaped like small screws or cylinders. These implants are surgically placed directly into the jawbone, where they function as a stable foundation for a replacement tooth. The procedure is highly successful and is used for a variety of cases, from single tooth replacements to securing full bridges or dentures. The success of endosteal implants relies on a process called osseointegration, where the jawbone naturally fuses with the implant over a period of several months, creating a bond as strong as a natural tooth root.
2. Subperiosteal Implants
Subperiosteal implants are an alternative for patients who do not have sufficient jawbone height or density to support an endosteal implant and wish to avoid a bone grafting procedure. This type of implant consists of a custom-made metal framework that fits directly on top of the jawbone, under the gum tissue. The frame has posts that protrude through the gums, to which the replacement teeth are attached. While less common than endosteal implants, subperiosteal implants can be a viable solution for those with a compromised jawbone structure.
3. Zygomatic Implants
Zygomatic implants are a highly specialized type of dental implants reserved for patients who have experienced severe bone loss in the upper jaw and would not be candidates for traditional implants. Instead of being placed in the jawbone, these implants are much longer and are anchored in the dense zygomatic bone (cheekbone). The procedure is more complex and requires a surgeon with a high level of expertise. Zygomatic implants provide an effective solution for full-arch restoration without the need for extensive bone grafting, significantly shortening the treatment timeline for a select group of patients.
The Dental Implant Procedure: Step-by-Step
Understanding the dental implant process can help alleviate any concerns and prepare you for your treatment journey. The procedure generally follows these key steps:
- Initial Consultation & Planning: The process begins with a comprehensive examination, including X-rays and 3D scans, to assess your oral health and jawbone density. A personalized treatment plan is then created.
- Implant Placement: The implant post is surgically placed into the jawbone. This is typically done as an outpatient procedure with local anesthesia.
- Osseointegration: This is the most crucial healing phase, where the jawbone grows around and fuses with the implant. This process can take several months, but it is essential for the long-term stability of the implant.
- Abutment Placement & Restoration: Once osseointegration is complete, a small connector (abutment) is attached to the implant. Finally, a custom-made crown, bridge, or denture is securely placed on the abutment, completing your new smile.
Benefits of Dental Implants
Choosing dental implants provides a range of significant benefits that are unmatched by other tooth replacement options. They look, feel, and function just like natural teeth, giving you the confidence to eat and speak without worry. They also prevent bone loss in the jaw, which can occur when a tooth is missing, thus helping to preserve your facial structure. With proper care, dental implants can last a lifetime, making them a wise and valuable investment in your oral health and overall well-being.